Adolescents living with HIV in Africa should be a priority population for health – and in particular mental health – interventions. The wellbeing of today’s youth will determine not only their future, but also our continent and region’s future and our ability to reach the United Nation’s Sustainable Development Goals by 2030.
Yet this future is currently looking fragile and challenged, given the many intertwined health and social problems faced by Africa’s youth. Africa is indeed a “youthful” continent: about 60% of the total population is under 25 years of age, according to the UN. Moreover, the continent’s youth population is predicted to rise more than any other region in the world, from an estimated 230 million in 2015 to 535 million by 2065. Africa is, sadly, also the continent that carries the highest HIV burden.
Of the 2.1 million adolescents living with HIV globally, about 1.7 million (84%) live in sub-Saharan Africa, according to the United Nations Children’s Emergency Fund (UNICEF). Additionally, African adolescents represent a growing proportion of people living with HIV, and the only population group for which AIDS-related deaths have increased over the past decade. As highlighted by UNICEF, this can be attributed largely to the fact that a generation of children who were infected with the virus at birth are now growing into adolescence.
As a 2014 study by Elizabeth Lowenthal and others reminds us, this trend is giving rise to challenges that will intensify over the next decade, especially in the sub-Saharan African region, where the ability of fragile health systems to reverse the epidemic and address the needs of life-long care and treatment will continue to be tested. A better understanding of the risk and protective factors for the health of HIV-affected adolescents is of critical importance if we are to develop responses aimed at protecting these young people’s wellbeing and survival.
This will require a holistic approach to health, in line with the World Health Organisation’s (WHO) definition, which sees physical, mental and social health as integral and inter-related components of a healthy life. Adolescence – defined by WHO as the 10-19 age range – is a challenging time in an individual’s life cycle, and this is true in any context or continent. It is a time of growth, change, exploration and experimentation, and as a result, also a time of particular health and mortality risks.
As highlighted in a WHO 2014 global report on adolescent health, adolescents are more likely to engage in substance use, sexual risks and other high-risk behaviours. UNICEF estimates that the proportion of adolescents with mental health symptoms is rising globally, with one in four adolescent children experiencing symptoms more than once a week. Depression is reported to be the leading cause of illness and disability among 15 to 19-year-olds globally, and suicide the first cause of death. These alarming figures are likely to be higher for African adolescents, many of who are also exposed to multiple social stressors such as poverty, violence and HIV. In particular, young adults living with HIV are likely to face what Lowenthal et al refer to as “recurrent and cumulative psychological stressors”.

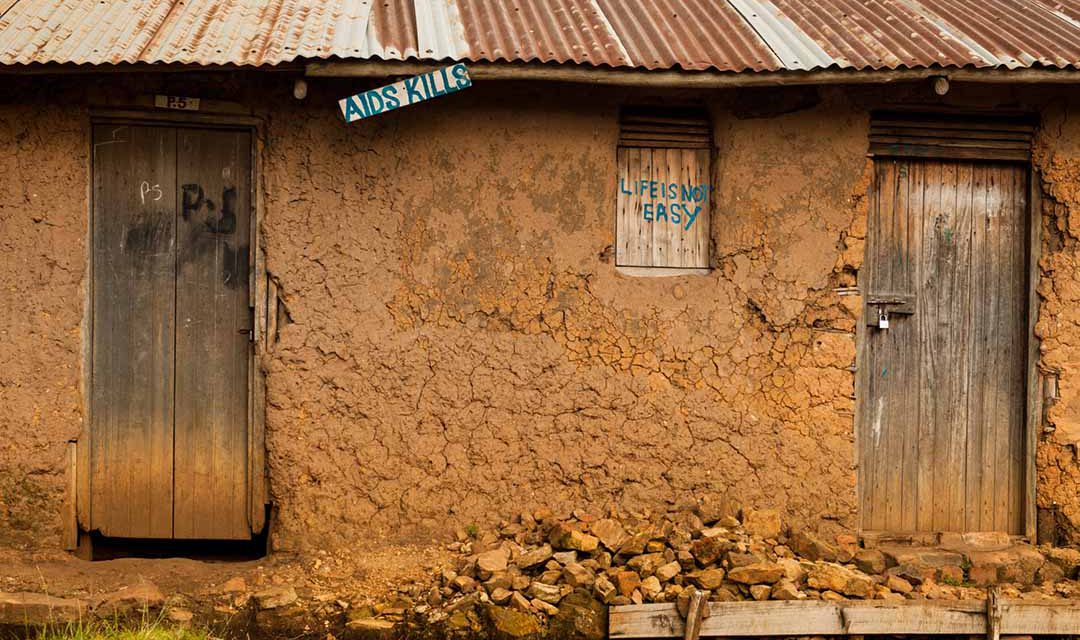
A sign of the times on a house in Uganda.
These include dealing with chronic illness, medicine adherence and the side effects of chronic medication while having to negotiate sexual relationships. In many cases, these adolescents also have to confront possible stigma, orphanhood and death in the family. Poor mental health can, in turn, be linked to many other factors in life, including poor quality of life, behavioural problems, worse educational outcomes, high-risk behaviours and lower retention in HIV treatment and care.
These may lead to increased rates of HIV transmission and AIDS-related illness and death. These risks, of course, extend beyond adolescence to an individual’s adult life and more broadly to society. As a 2017 UNICEF Research Brief indicates, mental health disorders can result in a health cost that is some 10 times higher during adolescence than during adulthood. They can also affect the ability to contribute positively to the economy and society later in life. The inclusion of mental health within the UN “Good Health and Wellbeing” Sustainable Development Goal for 2030 (SDG3 in the diagram below) arguably marked a long overdue turning point in terms of recognising the importance of protecting mental health.
However, mental health still remains relatively poorly resourced compared to physical health, with access to and uptake of mental health care services especially limited in low and middle-income countries. As I have argued in the past, we have also paid too little attention to the social component of health, the third key pillar of the WHO definition, which is very closely related to psychological wellbeing. While a common, widely accepted definition does not exist, “social health” can be taken to broadly refer to positive and beneficial interaction with other people and society at large.
A wealth of evidence links social interaction and relationships to better physical and mental health outcomes. According to a 2010 review by Julianne Holt-Lunstad et al, covering 148 studies conducted worldwide with 308,849 individuals, more or better-quality relationships are as important predictors of mortality as other well-established risk factors such as obesity and physical inactivity. “Social support” – defined as the “functional nature or quality” of social relations – is a key dimension in explaining the links between social relations and health. This refers to the emotional, informational and instrumental assistance that people need to stay healthy or adapt to stress. It can include such things as the availability of healthcare, information or advice, lifts to a health facility, and money or food, among others.
A large body of global research links social support to better mental health and lower odds of suicide, including among adolescent populations and individuals living with chronic illness. Yet very little large-scale empirical research has been done on the relationship between mental health and social support among HIV-affected populations in Africa, and evidence on effective interventions is even scarcer. This is even more so the case specifically for HIV-affected adolescents.
The research on social support and health that I have conducted over the past decade was motivated by the realisation of this gap, and the information I gathered while interviewing caregivers and children in rural and semi-urban HIV-affected South African communities over 2005-2009. Several caregivers of children – in some cases grandmothers taking care of multiple children of deceased or absent offspring – spoke of how important the help they received from their family and community was for their ability to cope, both emotionally and physically, with the many hardships they faced daily.
The first mixed-methods research I led on these themes was part of a larger South African health survey, the Young Carers project, a collaboration between Oxford and Brown universities, the Health Economics and HIV/AIDS Research Division (HEARD) at the University of Kwazulu-Natal, the South African government and other NGOs and research institutions. The study involved approximately 2,500 caregivers of adolescents living in communities highly affected by HIV. As reported in a 2014 article, my colleagues and I found that caregivers with more social support were less likely to experience anxiety and depression and more likely to have better self-reported physical health, as well as to practice more “positive” parenting.
These findings prompted me to start exploring the links between caregiver and adolescent support and wellbeing. In a subsequent analysis, published in 2015, I found that adolescent children of caregivers who received more social support were in fact less likely to have behavioural problems (for example, conduct problems, hyperactivity and emotional symptoms) and more likely to demonstrate pro-social behaviour (that is, behaviour intended to help others). However, better parenting approaches and better mental health of caregivers who were more supported only partially explained this phenomenon. My colleagues and I advanced a further hypothesis: that these adolescents may also have been receiving more support directly from individuals within the caregiver’s social network. We could not test this hypothesis in the 2015 study, but it was supported by subsequent qualitative work with a smaller group (24) of caregivers from this sample. Among other things, these caregivers believed that their adolescent children’s wellbeing was positively affected by the support they (the caregivers) received. This, they explained, was partly a result of their (caregivers) better psychological wellbeing, and better parenting and decision-making, which in turn had positive effects on their children’s lives. In addition, the children gained much information, encouragement and advice directly from individuals in the carer’s network.
More recent and on-going analyses, with 1,000 adolescents in the Eastern Cape who had initiated HIV treatment, have allowed me the opportunity to start looking at how social support received directly by adolescents living with HIV may affect their mental health and suicide risk. This work uses data from the Mzantsi Wakho project, a mixed-methods research project led by Oxford University and the University of Cape Town, which also involved part of the Young Carers research group.

Preliminary findings suggest that these adolescents on HIV treatment can be protected from depression and suicidal tendencies linked to experiences of stigma through social support provided by their social network, and participation in clinic support groups that provide informational and emotional support. This is particularly salient, since stigma is sadly still widespread among people living with HIV, with almost half of the adolescents in this study reporting some experience of being stigmatised. Moreover, adolescents who received more support from their social network appeared to be less likely to experience depression more generally, and therefore suicidal thoughts and behaviour. What reflections can we draw from these specific findings, as well as the broader research and context?
Firstly, it is clear that there can be no health without social health, just as there can be “no health without mental health”, as Martin Prince et al aptly put it in a 2007 article. Strengthening multiple support resources – for example by supporting existing mechanisms or relationships, or through health interventions – has the potential to promote better mental health and possibly facilitate service uptake among (HIV-positive and other) adolescents. This is not a magic bullet, but it is certainly a potentially key element within more multi-faceted interventions that aim to support young people across different domains.
Secondly, caregivers and other close family members play an important role in adolescents’ lives and health, and interventions need to take this into consideration. We have found that caregivers are often the main providers of emotional and tangible support for adolescents, and higher caregiver support has been linked to better adolescent mental health even among HIV-positive youth, as shown for example in a 2017 study by Shelene Gentz and others. This suggests that boosting the support received by caregivers of adolescents, as well as that directly received by the adolescents themselves, may have cumulative positive effects on adolescent health. It also suggests that it is important for adolescent health interventions to involve primary caregivers or other close adults in the child’s network, and/or work to strengthen child-caregiver interaction.
These may include initiatives such as community based parenting programmes. Several recent evaluations have, in fact, shown these programmes to be effective in reducing abuse and mental health problems among youth, even in low-resourced, HIV-affected African communities. Lastly, more applied research is needed to better understand the connections between the social, mental and physical dimensions of health, and to further develop and test health interventions in this specific adolescent population. We should draw from what we know works and is culturally appropriate and feasible in resource-limited African settings, including some of the initiatives mentioned above.
If we are to gain a better understanding of the needs of adolescents, we will need to make sure we involve adolescents in designing programmes developed for them. To best design and evaluate interventions, we need to be open to bridging academic disciplines and using methodological tools from different areas of study. We will also need to look for ways to increase the participation of key government and NGO stakeholders in initiatives such as those outlined above to ensure their sustainability – as well that of others that emerge from further study. As the UN’s 2015 Population 2030 report puts it:
“Adolescents and youth can be a positive force for development when they are provided the knowledge and opportunities they need to thrive.” Investing in the mental, social and physical health of Africa’s adolescents is essential if we are to provide them with opportunities to thrive and contribute to the African societies and economies of the future.